70M with multiple myeloma remission looking for alternative/unconventional therapy/dietary ketosis.
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
Patient:
'Here's a quick summary of my medical history that may be relevant to my condition:
'I'm a 70 year old mathematician/professor of computer science. I have worked on a number of medical projects with clinicians but have had no clinical training but I hope some understanding of some clinical issues.
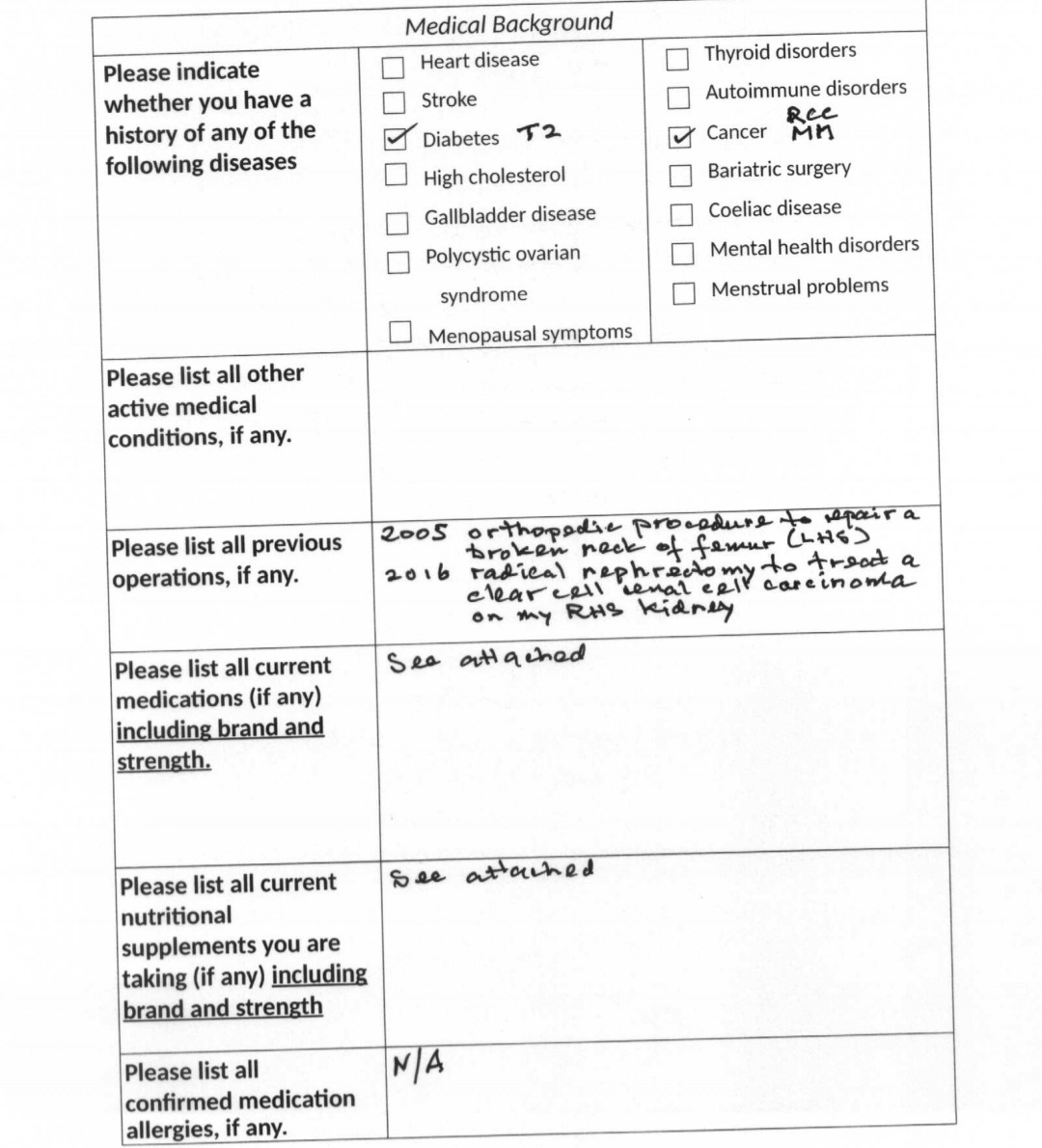
In 2005 I was diagnosed as a T2 diabetic which I was successfully controlling with a ketogenic diet ( eg my BGL in the morning before breakfast was 4 - 5 mmol/L before I had COVID in June 2022 after which it was consistently 2 mmol/L greater) before I started taking dexamethasone which has required me to have insulin injections to try and keep my BGLs at a reasonable level.
I was diagnosed with Clear Cell Renal Cell Carcinoma on my right kidney in the middle of 2016. I had a radical nephrectomy at the Royal B Hospital in early August 2016. This appeared to have worked as there has been no secondaries from the RCC since 2016.
After the above nephrectomy, I consulted a nephrologist, Dr O'S, to look after my remaining left kidney. She did an extension blood screen on me and copied my wife, Dr CM, who works as a GP in Brisbane. CM noticed the potential signs of MM in the blood test and phoned Dr O'S who hadn't seen the blood test results. They immediately contacted a haematologist, Dr R F, and organised for me to see her that Monday afternoon as I was due to fly to Dublin on the Friday of that week to attend the Advisory Board for an EU funded project to build a simulator for ultrasound guided peripheral nerve blocks. After a bone marrow biopsy and more blood tests I was diagnosed with MM on the Thursday :-(
When I returned to Brisbane from my European meetings, I went through chemotherapy for several months until I was ready for a stem cell transplant which took place in the middle of 2017.
Following the stem cell transplant I was effectively in remission until early last year. By March 2023, the level of my free light chains and paraproteins and other indicators were such that Dr F put me on Revlimid. The Revelimid was working ie reducing the concentration of paraproteins and FLCs so in July/August 2023 I went to the US and Canada to a conference at MIT and then the Conference in Los Angeles. Eventually, getting back to Australia for my father's 100th Birthday on August in Perth. A week later I returned to Brisbane, I became very sick with a very bad headache on the RHS of my head. I exhibited 6th nerve palsy and other nerve issues on the my RHS of my face.
I was admitted to GsPrivate Hospital to establish the root cause of what was happening to me. An MRI scan showed 3 lesions in my head:
one above my left eye between the skull and the dura,
my sinus and
my cavernous sinus.
At the time my clinicians strongly suspected they were plasmacytoma but they wanted to get a sample so that lab tests could confirm their suspicion rather than possibly related to my RCC from 2016.
My neurosurgeon, Dr SO, did a craniotomy and got a sample of the lesion above my left eye unfortunately the lab results were inconclusive as to whether it was a plasmacytoma.
Next my ENT surgeon, Dr W, inserted an endoscope up my nose and obtained a sample of the lesion in my sinus. The lab tests were conclusive - it was a plasmacytoma from the MM.
It was then decided to treat the lesion in my cavernous sinus using 5 short doses of x-rays - this worked well for all of the nerves running through the cavernous sinus except for the sixth nerve which is still a problem but fortunately it is improving slowly and I might have a complete recovery of my vision so that I can drive a car again!
I'm now on a 4 week cycle of dexamethasone+carlifozimib+pomalidomide. It started as Dex+Carlif but the blood tests dramatically improved once pomalidomide was added.
3 weeks ago I contracted a bacterial sinus infection and was admitted to G×××× Hospital. I was scanned which showed that my left clavicle bone had been fragmented by a plasmacytoma. This was treated with 5 doses of radiation.
Next week(Feb 28,2024) I'm due to have an FDG PET scan to understand better what's happening with the plasmacytoma. One course of action that's being considered by Dr F is another stem cell transplant with my remaining stem cells that were harvested in 2017'
-Multiple Myeloma was in remission for 7 years but came back with vengeance in August 2023.He made a trip to Delhi(while on chemo) to purchase Pomalidomide for his treatment for 3months supply that costs less than 1 month supply in Australia plus airfares,as it wasn't subsidised in Australia.After 2months of triple therapy,myeloma will be staged again and he will have a second stem cell transplant or have to look at other options if he is now in remission.CAR T cells or similar would be probably next options.He had metastatic plasmacytomas,myeloma to cavernous sinus and bone marrow proliferation.Anyhow,despite chemotherapy being awful,he has been rescued and currently faces uncertain future and exploring any alternative/conventional therapies.
It's been very tough lately as his wife CM has been diagnosed with Idiopathic pulmonary fibrosis because of anaesthetic complications during her hip replacement last December'
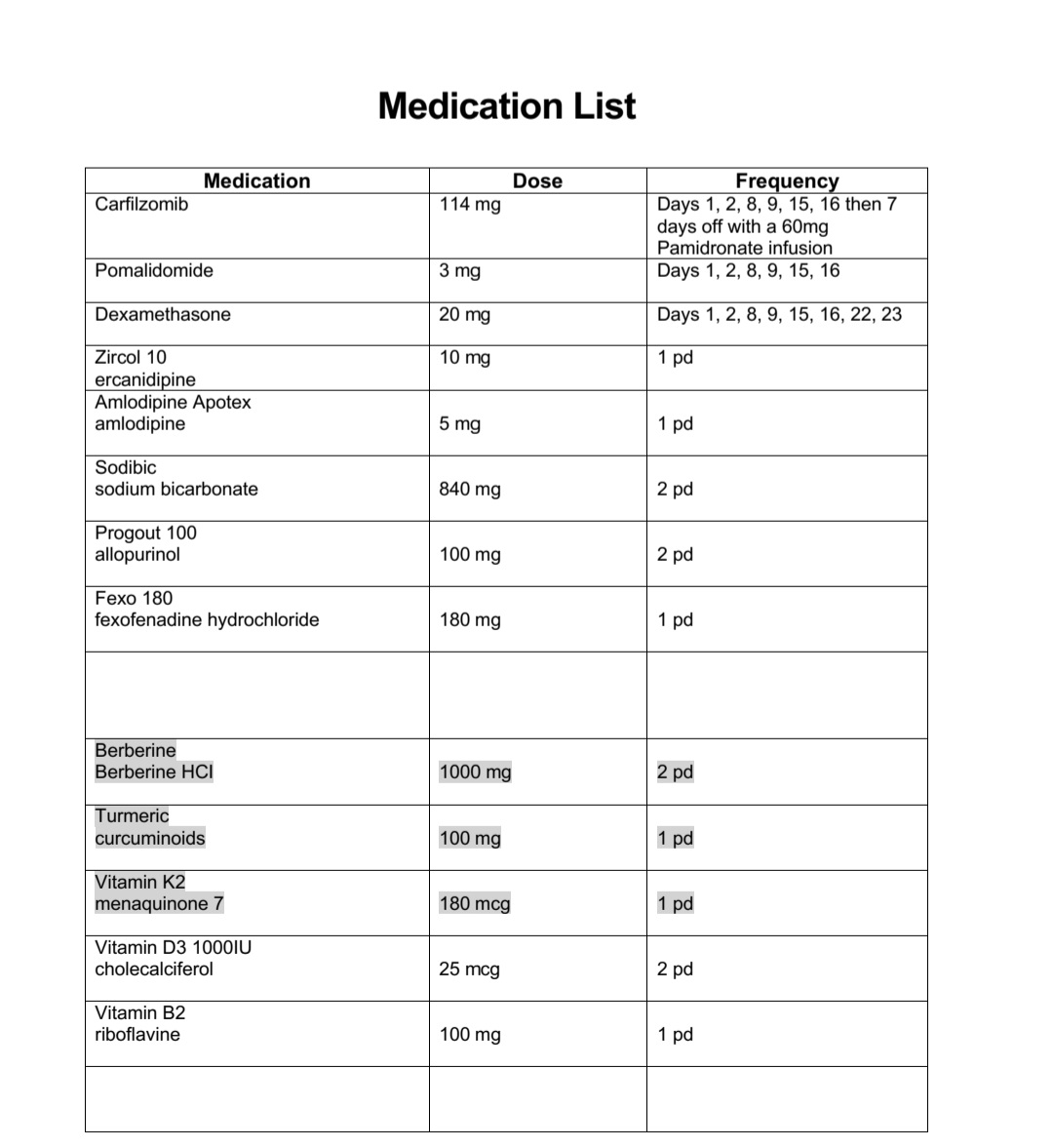
Current medication list
Current patient requirements.
-Wants to explore any alternative/unconventional therapy options.
Some other conversational inputs
'[25/02, 9:07 am] : Hi Dr.Dinesh, I'm back in Brisbane waiting to see my haematologist and then get treatment this afternoon: dexamethasone + carlifizomib. I took 3 mg of pomalidomide this morning. Yesterday went basically as I expected with Dr A P. The use of stress-pulse therapy with blood cancers is very new. A sent me this link which I need to go through https://careoncology.com/the-coc-protocol-and-blood-cancer/
Basically, the nutritional ketosis is achieved through <20 g of carbs, about 85 g of protein and the rest fat. I'll read through what A send me and send you any updates.
[25/02, 9:07 am] :
I'm finally feeling half normal today. Last Thursday and Friday I took 20mg dexamethasone each day which meant I got little or no sleep Thu/Fri/Sat but then on Sun/Mon I couldn't do anything but sleep all day/night. Unfortunately, this has been my usual pattern over the last few months of chemotherapy - so Tue/Wed are the only days when I feel half normal like when I saw you last week.
I met with Dr F last Thu and proposed exploring nutritional ketosis - she was less than enthusiastic and said that it wasn't considered an accepted clinical pathway.
I still want to go ahead but in three steps:
adopting a "low carb" diet that will better manages my BGLs on non-dex days (I definitely want to get my BGLs to lower levels without insulin, they're too high at the moment)
modifying the diet to better manage my BGLs during my dex days
and when the time is right going into full ketosis
If I undertake the first two steps without using the word "ketosis" it shouldn't provoke either my haematologist or endocrinologist - my relationship with both goes back over 7 years.
Dr AP:happy to explore "low carb" instead of "ketosis". the 2nd term seems
scary to some docs.
However any meaningful ketosis would be pretty hard with high dex dosing
- that is going to be the issue.'